Large language models like GPT can read guidelines, summarize clinical papers, and turn symptom lists into plausible differentials in seconds. That can feel like magic—especially at 2 a.m., when you’re worried and searching for answers. But medicine isn’t just pattern matching; it’s responsibility, uncertainty, and consequences. This article lays out what GPT can do well in healthcare, where it fails, and how to use it safely as a supporting tool—never a substitute for a qualified clinician.
What GPT is good at: comprehension, structure, and speed
GPT excels at transforming messy inputs into organized outputs. It can summarize discharge notes into plain language, structure medication lists, turn lifestyle advice into a weekly plan, and translate clinical jargon into terms a family can understand. It can also generate checklists for pre-visit questions, outline rehabilitation exercises from reputable sources, and draft consent explanations you can review with your doctor.
Early triage (with guardrails): helpful framing, not diagnosis
For symptom descriptions, GPT can produce a ranked list of possible causes with “red flag” warnings that indicate when urgent care is needed. Used correctly, this narrows the conversation and helps you prepare for an appointment. Used incorrectly—as a final answer—it can mislead, because the same symptoms map to very different risks in different ages, geographies, and histories.
Clinical research copilot: faster reading, better questions
Doctors and patients alike drown in literature. GPT can summarize papers, compare guidelines, extract inclusion/exclusion criteria, and highlight what evidence is strong versus speculative. It can draft a “questions to ask your specialist” list tailored to your condition, so limited appointment time focuses on the highest-value decisions.
Why relying on GPT alone is dangerous
Medicine depends on context (vital signs, exam findings, imaging, labs), bias awareness, and accountability. GPT doesn’t examine you, cannot order tests, and may confidently state an out-of-date or misapplied recommendation. It can also miss rare but critical conditions that a trained clinician is primed to catch, or overfit to common benign explanations when urgency is required.
Hallucinations and outdated advice
LLMs sometimes “invent” facts, citations, or contraindications. Even when accurate, recommendations may lag current guidelines or ignore country-specific standards. This is tolerable for meal planning; it is unacceptable for anticoagulation thresholds or pediatric dosing.
Privacy and data sensitivity
Your health history is among your most sensitive data. Before sharing, strip identifiers, minimize details, and understand how your data is stored, processed, and retained. Prefer tools that offer explicit privacy controls, local processing where possible, and clear deletion options.
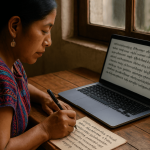
GPT as a health literacy booster
Used correctly, GPT can improve comprehension: explain an MRI report in plain language, outline pros/cons of treatment options, translate discharge instructions, or prepare a medication reconciliation sheet. Greater literacy supports shared decision-making and adherence—two pillars of better outcomes.
Safe usage pattern: prepare → ask → verify → act (with a clinician)
Come to GPT with a concrete goal (e.g., “prepare for my asthma review”). Ask it to list key questions, guideline checkpoints, and home-monitoring metrics. Take those notes to your clinician. After the visit, use GPT to recap the plan in your own words and generate reminders or trackers you’ll actually follow. Verification sits with the clinician; GPT helps you organize and remember.
How to prompt for safer medical outputs
Be specific about age, relevant history, meds, and timing, but ask for ranges and uncertainty notes. Request explicit “do not diagnose—provide differential with risk levels and red-flag criteria for urgent care.” Ask for source types (e.g., “major guidelines,” “systematic reviews”) and for the model to note when evidence is weak or dated.
Red flags: when to skip GPT and seek urgent care
Severe chest pain or pressure, signs of stroke (face droop, arm weakness, speech difficulty), severe shortness of breath, uncontrolled bleeding, head injury with loss of consciousness, new confusion, high fever with stiff neck, sudden severe headache (“worst ever”), suicidal thoughts, or anaphylaxis symptoms. In these scenarios, do not chat—call emergency services or go to the nearest emergency department.
Chronic conditions: where GPT can help between visits
For diabetes, hypertension, asthma, or chronic pain, GPT can help build self-management routines: log templates, symptom diaries, diet frameworks, and exercise schedules that respect your limitations. It can also suggest evidence-based behavior change techniques (implementation intentions, habit stacking) and reminders phrased in ways you find motivating.
Medication safety: double-check with a pharmacist or clinician
GPT can list common interactions or side effects, but final decisions require a professional who knows your full profile and the latest formularies. Use GPT to generate a concise medication list with dosages and timing, then review that list during appointments. Never start, stop, or change a dose based solely on chatbot advice.
Mental health: language can support, not replace care
GPT can offer coping strategies, journaling prompts, psychoeducation, and crisis resources. But it cannot assess risk in real time or provide therapy. If you are in crisis or considering self-harm, contact local emergency services or a trusted crisis line immediately. Treat GPT as adjunctive self-help, not treatment.
For clinicians: workable ways to integrate GPT safely
Use GPT to draft patient education materials at different reading levels, summarize long chart histories, generate differential checklists you then prune, or propose templated after-visit summaries. Keep it out of final medical decision-making: your judgment, documentation, and accountability remain central.
Documentation hygiene and bias checks
Ask GPT to list uncertainty, alternatives ruled out, and potential biases (“anchoring on prior label,” “availability bias from recent case”). This can improve your note quality and self-audit. But ensure protected attributes are handled appropriately and that outputs don’t propagate stereotypes or inequities.
Second opinions and shared decision-making
Patients often leave with partial recall. GPT can restate options with risks, benefits, and “what matters to you” questions, helping families hold a better conversation before committing. Bring those notes back to your clinician for alignment rather than treating them as verdicts.
Building a personal health knowledge base
Keep a simple, private document with conditions, surgeries, allergies, meds, vaccine dates, and baseline lab values. Use GPT to format it cleanly and maintain a one-page summary for emergencies. Updated, portable information reduces errors across different care settings.
What the future may bring (and what must not change)
Expect tighter integration with wearables, home diagnostics, and clinical systems, enabling models to flag trends and nudge timely follow-ups. But two essentials should remain: clinician oversight for decisions and patient consent for data use. Speed and convenience cannot replace accountability and trust.
Bottom line: GPT is a capable assistant, not your doctor
Use GPT to understand, organize, and prepare. Use clinicians to diagnose, treat, and decide. If advice from GPT conflicts with medical guidance—or your condition worsens—defer to qualified care immediately. Responsible use pairs AI’s strengths (clarity, structure, speed) with human judgment (context, ethics, accountability) to keep you safer and better informed.
Conclusion
It is reasonable to consult GPT about your health; it is risky to rely on it. Treat the model as a health literacy tool and planning aid that helps you ask sharper questions, remember instructions, and stay organized. Keep final decisions with licensed professionals who can examine, test, and follow up. That partnership—curious patient, supportive AI, accountable clinician—is the safest way to bring intelligence into care without losing the human heart of medicine.


GPT can make health info clearer and prep you for better conversations, but it should never replace real clinical judgment 💯